
Since the introduction of fast diagnostic tracks in many areas of oncology, the traditional processing of bone marrow biopsies (BMB), requiring either resin embedding or lengthy fixation and decalcification, is due to an upgrade. Thanks to a growing number of new commercially available tissue processors, microwave-enhanced processing is becoming a standard tool in the pathology laboratory, allowing rapid fixation and decalcification of BMB with preserved morphology and antigens. In this short report, we describe the use of a commercially available EDTA-based decalcification fluid (USEDECALC, Medite, Orlando, USA) in combination with the LOGOS J (Milestone, Bergamo, Italy), a closed microwave-enhanced tissue processor, for overnight fixation, decalcification, and paraffin impregnation of the BMB. This allows next-day reporting without impaired morphology or immunohistochemistry, and even improved DNA quality of the BMB.

Avoid common mistakes on your manuscript.
Many systemic diseases, including auto-immune and infectious diseases, but also various malignancies present or originate in the bone marrow. Despite developments in immune flow cytometry and molecular diagnostics of blood and bone marrow, the trephine bone marrow biopsy (BMB) remains a crucial diagnostic, staging, and prognostic tool in hematopathology. Immunohistochemistry and molecular techniques on the BMB complete traditional morphology [1, 2], requiring preservation of antigens, DNA, and RNA. Due to the growing importance of single day stays in the outpatient clinics, the pressure to shorten turnaround times of BMB increases. This requires redesigning the process of fixation and decalcification of BMB, which traditionally required up to 5 days.
The combination of the hard, bony structures, and the enclosed delicate cells with many different nuclear and cytoplasmic structures, containing enzymes that have to be preserved, make processing of BMB a challenge. Over the years, various fixatives have been developed to improve morphology or speed up the fixation from the traditional 24–48 h required with standard formalin, but these fixatives are not necessarily suitable for immunohistochemistry and molecular techniques. Therefore, formalin-based fixatives are still preferred in most pathology laboratories. Although resin embedding allows cutting of the bone with optimal preservation of cytological details, decalcification followed by paraffin embedding is nowadays mostly preferred, since the loss of cellular detail by decalcification can be compensated by cytomorphology of the aspirate, supplemented with immunohistochemistry on the BMB.
Both decalcification and resin embedding slow the processing of BMB considerably, requiring up to two additional days. Acidic fluids such as formic acid were introduced to speed up the decalcification process, however, compromising morphology, immunohistochemistry, enzyme reaction, and DNA/RNA quality. As an alternative, 24- to 48-h formalin fixation, followed by ultrasound [3] or microwave [4] accelerated decalcification in EDTA, was introduced, leading to an improved turnaround time and good diagnostic quality. We further improved our previous BMB protocol to reach a turnaround time of 2 days (Table 1) with equal morphological, immunohistochemical, and DNA quality.
Traditionally, we have used Burkhardt’s fixative, a 12 % buffered formaldehyde solution supplemented with methanol and glucose, for many years because of the better morphology than achieved with buffered formaldehyde alone, when using our previous protocols. We still receive the BMB in Burkhardt’s, but the current protocol is performed after exchanging this fixative for buffered formaldehyde.
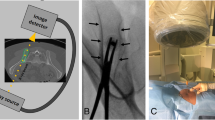
The BMB are then processed in the LOGOS J (Milestone, Bergamo, Italy), a fully automated system that performs microwave-enhanced fixation, decalcification, and paraffin impregnation in a closed system. This enables overnight protocols (Table 1). For rapid decalcification, we use a chelating, EDTA-based solution (USEDECALC, Medite, Orlando, USA). Compared to other commercially available decalcifying solutions that we have tested, this gave the best results for morphology and DNA yield. Another important factor that determines the results, notably of the Leder (chloracetate esterase) stain since this requires an intact enzyme, is the maximum temperature that is used during the whole processing. Restricting the temperature to 60 °C allows enzyme stains (Fig. 2c; Leder staining) with a slightly better contrast than with our previous protocol. The technical details of the program are presented in Table 2.
We optimized different steps of our decalcifying protocol during the past years to arrive at our current protocol. Indeed, alternative agents for rapid decalcification at room temperature with acceptable DNA and RNA results have been reported. These are mainly combinations with 14 % EDTA or formic acid (for example, Formical-4 (formic acid/EDTA/formaldehyde, Decal Chemical Corporation, Tallman, NY), Formical-2000 (EDTA/formic acid, Decal Chemical Corporation, Tallman, NY), Immunocal (formic acid, Decal Chemical Corporation, Tallman, NY), and Surgipath Decalcifier I (formic acid/methanol/formaldehyde, Leica Biosystems) [6]). On the other hand, hydrochloric and nitric acid-based agents are not recommended or show clearly worse results in several studies (for example, Nitrical (nitric acid, Decal Chemical Corporation, Tallman, NY), IMEB (HCL/formic acid, IMEB, San Marcos, Calif), Surgipath Decalcifier II (HCL/EDTA, Leica Biosystems), Overnight bone decal (EDTA/HCL, Decal Chemical Corporation, Tallman, NY), Decal Stat (HCL/EDTA, Decal Chemical Corporation, Tallman, NY), and RDO Gold (Hydrochloric acid based, Apex Engineering Products Corporation, Aurora, IL) [6, 7]).
In conclusion, by adjusting our protocol for the processing of BMB, we successfully reduced the processing time of BMB, allowing sign-out within 24 h of receipt of the biopsy without compromising the quality of morphology and antigen detection and improved DNA quality.